Which income protection plans include hospitalisation benefit?

In reading this article, you will understand:
- What is meant by the term ‘hospitalisation benefit’ and why might it be necessary
- When does the benefit start paying and for how long
- Whether hospitalisation benefit is worth having
Income protection plans are designed to pay a replacement income if the client is incapable of working due to ill health, however insurers increasingly are offering a lot more in the way of additional support. This could take the form of numerous benefits and services to help the client maintain their health and wellbeing or seek professional advice for more minor, everyday ailments. In some cases that support can also come in the form of additional payments during the deferred period to provide financial assistance in certain circumstances. One such feature offered by a few income protection providers is hospitalisation benefit.
What is hospitalisation benefit?
Hospitalisation benefit is a policy feature where the insurer will pay the client a fixed daily benefit if they are hospitalised for a certain number of days, during their deferred period. It is intended to provide financial support whilst the client is in hospital and not yet in receipt of their core monthly IP benefit payments.
Because hospitalisation benefit is paid during the deferred period (i.e. after a claim has been submitted), the client will in most cases need to meet the insurer’s incapacity definition and be medically incapable of performing their own occupation. If the client is discharged from hospital and returns home for care or recovers and returns to work, then the benefit will cease.
Why might hospitalisation benefit be necessary?
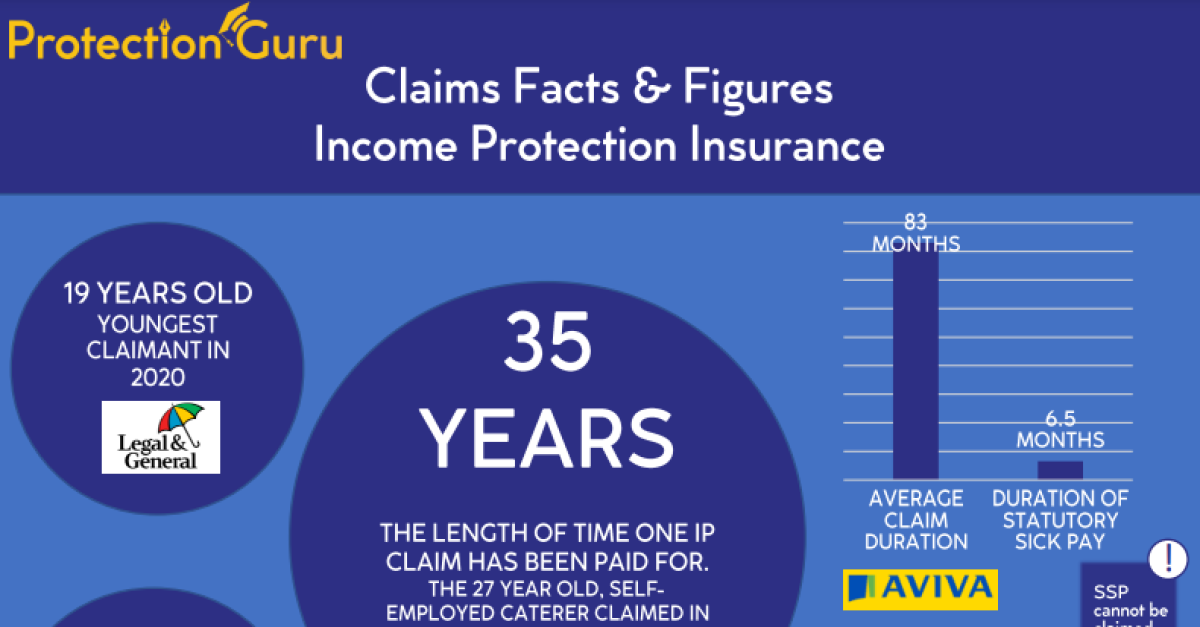
All income protection policies will have a deferred period and whilst some insurers offer very short deferred periods of just 1 day (referred to as ‘back to day 1’, but usually requiring the client to be off work for 3 days before kicking in), most policies arranged will have a deferred period of at least 4 weeks or more. This means the client will need to support themselves financially for this initial period of a claim, either through employer sick pay, state benefits or their own savings (especially so if they are self-employed and without access to employer sick pay).
Whilst in many cases the policy deferred period will be selected to align with the client’s sick pay or however long their savings could sustain them, often the cost of the policy will also be a factor in determining the deferred period. As a rule of thumb, the longer the deferred period the lower the monthly premium, so it can be one way of reducing the cost of the policy for clients who are working to a budget. In doing this though, these clients are extending the amount of time that they will need to financially support themselves should a claim arise, which could be problematic.
Because hospitalisation benefit is paid during the deferred period, albeit not necessarily for the full duration as we’ll see below, the client has access to financial support immediately that can help with their bills and living costs. It’s a benefit that’s worth being aware of therefore, because when offered this can form part of any deferred period considerations.
Who offers hospitalisation benefit?
Insurer |
Hospitalisation Benefit Included? |
British Friendly |
No |
Ciencester Friendly |
Yes |
Guardian |
Yes |
Holloway Friendly |
No |
Legal & General |
Yes* |
Royal London |
Yes |
The Exeter |
No |
Vitality |
Yes |
Zurich |
Yes* |
IMPORTANT
Hospitalisation benefit is not included on the following products from these insurers:
Legal & General: Low Start IP
Zurich: Core
In most cases, the hospitalisation benefit is a contractual benefit. This means it is part of the terms and conditions of the contract, so the insurer is legally obliged to continue providing it for the duration of the contract. Only Cirencester Friendly do not offer hospitalisation benefit on this basis. This means the benefit is provided at the insurer’s discretion, so they can remove it at any time.
In Cirencester Friendly’s case, hospitalisation benefit forms part of their My Extra Benefits and costs £4 per month (combined with a fracture benefit)
It is the only insurer in our table that structures the benefit this way. However, the flip side of charging extra for this benefit is that Cirencester Friendly can pay hospitalisation benefit sooner than the other providers.
When is hospitalisation benefit paid?
To be eligible for the hospitalisation benefit payment, the claimant must spend a certain number of consecutive nights in hospital before the benefit is paid.
Guardian are worth highlighting because unlike everyone else, from the 7th night in hospital they will back-pay the benefit from the 1st night in hospital. This means that as long as the client is in hospital for more than 6 nights, they are covered from the 1st night they end up in hospital and would therefore potentially receive a higher pay-out overall.
How long is hospitalisation benefit paid for?
Apart from Cirencester Friendly and Legal & General, the hospitalisation benefit is paid until the deferred period ends but up to a maximum of 90 nights (84 nights for Legal & General). Clients with a deferred period of 6 or 12 months therefore will only receive the hospitalisation benefit for the first 3 months of their deferred period.
Cirencester Friendly are slightly different in that they pay the hospitalisation benefit for a maximum of 21 days. This aligns though with their client demographic of more manual workers and tradespeople, with shorter deferred periods.
Is hospitalisation benefit worth it?
This is a question that’s worth asking, because although apart from Cirencester Friendly, none of the insurers charge extra for it, the cost is still factored into the overall premiums clients are paying for the policy. It’s also an important question to ask if hospitalisation benefit is one factor in driving a product recommendation.
In many cases a hospital is not an appropriate setting for patients to recover in following an illness or surgery and in some cases capacity pressures and the need to free up bed space may result in patients being discharged earlier than in the past.
Research published by Health Org highlights that the average length of a hospital stays increased from 7.3 days in 2019 to 8.3 days in 2022 (13%). Length of stay for emergency admissions grew from 7.9 to 9.1 days (15%), while length of stay for elective admissions decreased slightly from 5.2 to 5.1 days (3%).
These stats and numbers of course do not tell the full story and there will be many people who have a lengthy hospital stay. We have therefore gone out to those insurers who offer this benefit to gather some case studies and stories, to better understand the usefulness of hospitalisation benefit and the impact it has had when it has been claimed on. We will publish these findings in a separate future insight.
Overall, all insurers have their merits. Just comparing each insurers offering as far as the benefit is concerned, Guardian, Royal London, Zurich and Vitality deserve a mention for ticking most of the right boxes. They all provide hospitalisation benefit as a contractual benefit and pay £100 (£150 in the case of Guardian) a night up to a maximum of 90 nights. Guardian perhaps deserve extra credit, because they will back-pay from the 7th night, therefore ultimately paying out a higher amount for shorter claims. Where the benefit is high, it is likely that Legal & General will pay more as the amount they pay is linked to the benefit.
Arguably, to some extent the Cirencester Friendly offering is strong as well because the benefit is paid after 3 nights rather than 6 or 7 as is the case with everyone else. Just going on the current average length of hospital stay stats highlighted above, Cirencester are potentially more likely to pay out than anyone else.
It’s also worth mentioning Metlife who, although not a traditional income protection policy, offer hospitalisation benefit as part of their core cover proposition paying up to £250 per 24-hour period clients are in hospital due to an accident from day 1. If the client is hospitalised due to sickness up to £250 per 24 hours from day 1 will be paid after the policy has been in force for a minimum of 12 months. The amount paid will depend on the number of units bought as follows:
Number of Units |
Daily Payment |
1 Unit |
£50 |
2 Units |
£100 |
3 Units |
£150 |
4 Units |
£200 |
5 Units |
£250 |
Things to reflect on for CPD:
- How could you adjust your approach with clients, to have a more meaningful conversation on this topic?
- Is there scope in the market to have hospitalisation benefit as a standalone benefit (like fracture cover or Children’s CI) which can be added to any protection insurance product, to allow those unable to get income protection a safety net in case of hospitalisation?