How our independent medical panel benchmark critical illness wordings

Even with the recent trend of simplification critical illness wordings are complex. Most definitions will include detailed medical terminology which will mean very little to most. Whilst some definitions from insurers may look very similar, an “and” instead of an “or” can make a massive difference in coverage. It is our belief that only those that practice medicine have the necessary skills to compare the precise wording of such policies. Consequently our critical illness benchmarking as deployed in ProtectionGuruPro service or in the iPipeline Product Features report is carried out by a highly qualified panel of doctors. In this article we highlight the process our doctors go through when benchmarking Critical Illness plans and how they provide an overall comparison of insurer coverage based on your client’s specific scenario.
In simple terms there are two aspects to our doctor’s critical illness benchmarking, which when combined enable us to provide an overall score for each client highlighting what plans are more likely to pay a claim. Importantly this analysis takes no account of an insurers claims philosophy. It is solely based on their wordings and as such what they are contractually obliged to pay out on. The two aspects of our benchmarking are:
- Scoring of each condition for each product based on the likelihood of a client being able to claim.
- The likelihood of a client suffering from each condition based on their age, gender and smoker status.
Below we explain how each aspect works and how they are combined to provide an overall score:
Likelihood of being able to claim on a condition by conditions basis
When assessing each insurer’s definitions our doctors will give each product a score between 0 (no credit) and 100 (highest score) for each condition analysed.
A score of 0
There are two ways an insurer could be given a score of 0 and therefore get no credit for a certain condition. The first, and most obvious, is if they do not offer a definition for the condition and therefore are not covering it.
An insurer could however, provide a definition for a certain condition and still score 0. This could happen where they have certain stipulations within their wording which, when assessed, our doctors have concluded that what they are asking for would never actually happen. One example of this is “Carcinoma in situ of the colon or rectum” as our doctors explain:
“Incidence rates are not unsubstantial, with 3,189 cases registered through the English cancer registry in 2017. Early cancers may increase further due to the recently commissioned NHS bowel scope screening programme. This involves a camera investigation at the age of 55 to look inside the bowel and to remove any small growths, called polyps, that may eventually turn into cancer. This should hopefully result in lower rates of cancers progressing to the more severe later stages and higher rates of early pre-invasive cancers.
The following is an example of one insurer’s wording:
Carcinoma in-situ of the colon or rectum diagnosed with histological confirmation by biopsy together with the undergoing of surgery to remove part of the colon or rectum. For this definition, the following are not covered:
– Treatments including local excision or simple polypectomy
The wording states the requirement for histological confirmation. Histology is where a pathologist looks at a sample of tissue, often referred to as a biopsy, under a microscope. This occurs whenever tissue is removed from a patient to help clinicians come to a diagnosis and work out the best form of treatment.
In the colon and rectum, there is an ongoing worry that the term “carcinoma in situ” may lead to unnecessary surgery being performed when there is no evidence to show a potential for the cancer to spread until it has grown through the basement membrane into the muscular layer. The Association of Coloproctology of Great Britain and Ireland noted in a position statement in 2013 that “carcinoma in situ” should no longer be used and that pathologists should be actively discouraged from using this term to reduce risk of over treatment.
This policy has continued to the present day, as demonstrated by a recent Public Health England guideline written for pathologists working in the NHS bowel cancer screening programme. Again, this clearly discourages the term “carcinoma in situ”, suggesting that the term high-grade dysplasia be used in its place. This makes a positive histological diagnosis of carcinoma in situ of the colon by a UK based pathologist increasingly less likely, and would be going against current good-practice guidance.
With this stipulation in place, it would be hard to see how a customer is likely to achieve a successful claim from this wording and therefore this has been scored 0%.”
A score of 100
As with a score of 0, there are two ways that a product can achieve the top score of 100 for a given condition. As might be expected, any wording that requires diagnosis only is given a score of 100 as anyone diagnosed with the condition should be able to claim.
An insurer might also stipulate a certain method of diagnosis, surgery or treatment type and still achieve a score of 100 as our doctors believe that what the insurer is asking for would always happen and therefore the client should always be able to claim. An example of where this might happen is some insurers Multiple Sclerosis definitions as our doctors explain.
“On occasion, simplicity can lead to receiving the best score for a wording. There is a growing trend for insurers to simply specify the requirement for a diagnosis by a consultant hospital specialist. This has additional benefits, as it allows for the rapid changes and advancements that are occurring in medical care. If a specific treatment or diagnostic investigation is stipulated in an insurance policy, this will be set in stone for the life of the policy and affect its future value.
For example, with multiple sclerosis (MS), one insurer’s wording is:
A definite diagnosis of multiple sclerosis by a consultant neurologist. There must have been clinical impairment of motor or sensory function caused by multiple sclerosis.
Which can be compared with another insurer’s:
A definite diagnosis of Multiple Sclerosis by a Consultant Neurologist. There must have been clinical impairment of motor or sensory function together with positive findings on Magnetic Resonance Imaging (MRI).
The first wording has been scored 100%, as MS will be diagnosed through a neurologist and an impairment of motor or sensory function is a prerequisite to it being diagnosed. The second wording has the additional requirement of an MRI scan.
All patients being investigated for MS should have a brain MRI with and without contrast. There are cases where the MRI scan is inconclusive and supporting evidence from additional tests must be relied on, such as with lumbar puncture for cerebrospinal fluid-specific oligoclonal bands, visual evoked potentials, and/or optical coherence tomography. Therefore, this wording was given a score of 95%, as this is the reported percentage of MRI scans of the brain that are abnormal in patients with clinically definite MS.”
A score between 1 and 99
Clearly not all wordings will pay on diagnosis alone or cover all severities of a certain condition. As such there are many conditions that our doctors will give a score of between 1 and 99. The actual score an insurer achieves for a given condition will be based upon the statistical chance of a client meeting the criteria if diagnosed with a condition. To ascertain the precise score our doctors will study audits, disease registries and other medical literature to understand the percentage of people that will fit the given criteria when diagnosed with the condition.
When doing this, understanding the validity and context of this information is vital as it might be easy for someone that does not have medical qualifications to misconstrue the data.
One example of a condition where insurers scores vary significantly is Coronary Angioplasty as our doctors explain:
“Insurers definitions for many conditions have very similar wordings, with standardised phrasing used throughout. Coronary angioplasty, requiring Percutaneous Coronary Intervention (PCI), is different in this regard. There are many variations on insurers wordings, resulting in significant differences to scores.
PCI is a less invasive alternative to open heart surgery to treat coronary artery disease, where atherosclerotic plaques build up in the small blood vessels of the heart, blocking the blood supply. This is performed under local anaesthetic, with a small wire being inserted into an artery in the arm, wrist or groin and then guided up towards the heart using an X-Ray video. The blockage can then be corrected by a number of procedures, such as inflating a small balloon and squashing the blockage. A stent is also often left in place to keep the artery open.
This is a surgical intervention with high incidence rates. The British Cardiovascular Intervention Society (BCIS) registry in 2016 published rates of 153 per 100,000 of the population per year. The overall coverage for this condition in the critical illness insurance market is actually much lower due to cross coverage. PCI is a treatment used following a heart attack (accounting for 58.3% of all PCIs in 2016), and so this would be covered by an insurer’s heart attack wording. It is also documented that just over 25% of patients who have PCI have had a previous procedure (likely rendering them ineligible to a successful future insurance claim). Therefore, the incidences rates appropriate for a critical illness policy are closer to 45 per 100,000.
Insurers criteria can depend on a number of factors, including the degree or blockage seen on angiography, how many and which arteries are affected, a mixture of the two, or the type of procedures used. Below is a table which documents some of the major differences in criteria that exists between recent wordings for this condition:
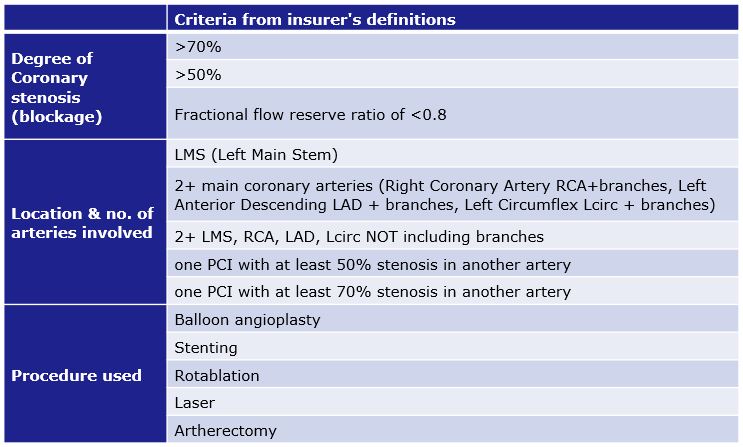
From current audit and disease registries, it is possible to provide accurate scores for each of the insurers wordings. Therefore, comparing the best and the worst in the current market, the best definition scores 100% as it gives no additional stipulations in its wording:
PTCA or other percutaneous coronary artery procedures performed by a Consultant Cardiologist to dilate and treat a coronary artery stenosis. The procedure may or may not involve the use of a stent.
Compared to another policy, which has multiple stipulations and significantly reduces the likelihood of a successful claim, and scores only 23%:
The undergoing of balloon angioplasty, including atherectomy, laser treatment or stent insertion on the advice of a consultant cardiologist to two or more main coronary arteries to correct narrowing or blockages. The main coronary arteries for this purpose are defined as Right Coronary Artery, Left Main Stem, Left Anterior Descending and Circumflex. Angiographic evidence will be required. Two coronary angioplasty procedures performed in different arteries at different times is covered. The following are not covered: • Diagnostic angioplasty • Two angioplasty procedures to a single main artery or branches of the same artery.
Likelihood of suffering from a condition
Understanding which policies offer broader coverage on a condition by condition basis is great, however in order to understand which policy might offer better coverage overall we need to know what conditions the client is more likely to suffer from. In doing this we can weight each condition based on the chances of the client suffering from it, with the conditions they are more likely to suffer from having a bigger impact on the overall score, the conditions they are less likely to suffer from having a lesser impact and the conditions they cannot suffer from having no impact.
To do this we use incidence data. This tells us the number of people in the population that are diagnosed with the condition in a given year (usually x in 100,000). To provide even more accurate weightings the incidence data our doctors have obtained is also:
- Gender specific – To highlight the differing likelihoods of males and females suffering from conditions and to ensure that where a certain gender is unable to suffer from a certain condition this is not weighted.
- Age banded – Giving us the specific incidence at different age ranges (usually in 5-year intervals i.e. 15-19, 20-24, 25-29 etc.).
- Reflecting the risk of smoking – Our doctors have factored in the risks of being an ex or current smoker onto the incidence rates.
By collating this incidence data for each condition we are able to calculate a weighting for each which is based on the client’s likelihood of suffering from each condition during the term of the plan. Therefore if you are running an analysis for a 30 year old taking out a plan with a 20 year term we would calculate the likelihood of suffering from conditions between the age of 30 and 50. By combining this weighting for each condition with the individual scores our doctors have awarded a product for each condition we are able to provide an overall score.
This level of benchmarking is carried out every time an adviser uses our critical illness analysis. Clearly, these calculations are happening in the background and not seen, but advisers can rest assured that when using our critical illness benchmarking either on ProtectionGuruPro or iPipeline’s SolutionBuilder they have a panel of doctors’ expert analysis at their fingertips.