What is a Second Medical Opinion Service and who o...
Posted by Adam Higgs | Apr 18, 2024 | Added Value Benefits, Added Value Benefits, Added Value Benefits, Added Value Benefits | 0 |
Non-Medical Underwriting Limits on Income Protecti...
Posted by Adam Higgs | Apr 16, 2024 | Income Protection, Underwriting Limits | 0 |
Exciting Career Opportunity for a Protection Speci...
Posted by Ian McKenna | Apr 15, 2024 | Join the team | 1 |
How do critical illness plans cover parkinson̵...
Posted by Adam Higgs | Apr 11, 2024 | Critical Illness, Critical Illness Conditions, Critical Illness Conditions | 0 |
Which Insurers are adapting Income Protection for ...
Posted by Adam Higgs | Apr 10, 2024 | Deferred Periods, Income Protection | 0 |
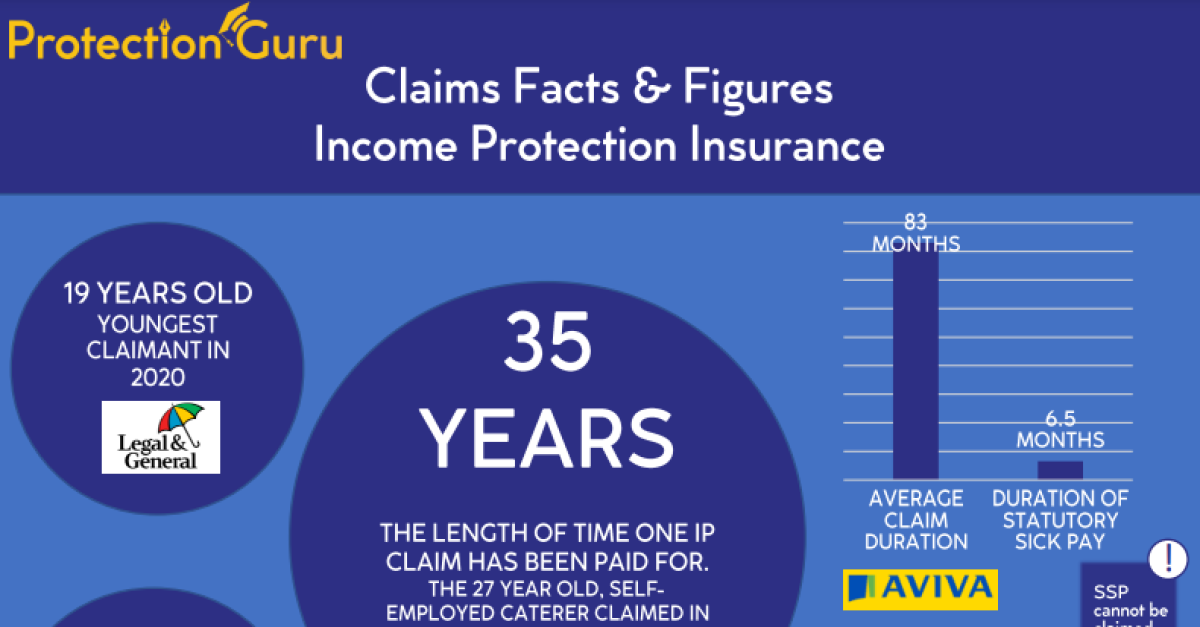
Individual protection underwriting limits – 4 things you should read
Apr 19, 2024
Understanding when and what medical evidence may be required when recommending a protection...
Read MoreExciting Career Opportunity for a Protection Specialist at Protection Guru
Apr 15, 2024
At Protection Guru, we’re on a mission to demystify the protection and life insurance industry....
Read More
×
User Details
Contact Us